
Blogs


DialaChemist announced as Cambrooke UK’s new home delivery service
DialaChemist announced as Cambrooke UK’s new home delivery service

For more information, contact us on ukinfo@cambrooke.com.

Depression & the PKU Diet
Living with PKU
Living with PKU is hard, you need to follow a very restricted low protein diet for life which may involve eating and drinking foods and protein substitutes that you may not like. Feelings of isolation, loneliness and embarrassment can start to develop as a result. Dr Gisela Wilcox at the Salford PKU event, recalled a PKU child asking if they ‘can eat human food now’ at their birthday, which demonstrates how different PKU patients can feel their entire lives as a result of following the PKU diet.
Eating out, and being spontaneous is so difficult that many people feel that staying and eating at home is the best plan of action to stay on their PKU diet. Many patients have also experienced being the only ones not invited to a birthday party, further distancing them from their peers.
What is depression?
Depression is the most predominant mental health problem worldwide. According to the NHS, most people go through periods of feeling down, but depression is when you feel persistently sad for weeks or months, rather than just a few days. Depression is a real illness with real symptoms, it isn’t a sign of weakness or something you can “snap out of” by “pulling yourself together”.
How to tell if you have depression?
Depression affects people in different ways and can cause a wide variety of symptoms including, but not limited to:
- Lasting feelings of unhappiness and hopelessness
- Losing interest in the things you used to enjoy
- Feeling very tearful
- Constant anxiety
- Constant tiredness
- Sleeping badly
- Having no appetite
- Various aches and pains.
These symptoms can be quite mild or very severe, or somewhere in between.
Low protein diet & treatment of depression
Treatment for depression is varied, and you should always consult a health professional who will guide you towards the right treatment for you. It is also important to understand the role of diet in this area.
Certain key nutrients (Vitamin C, Vitamin B12 and Folate (Folic acid)), which can only be obtained through diet, are involved in the making of chemicals called Biopterins. These play a significant role in the synthesis of a number of chemical messengers in the brain called neurotransmitters, including dopamine and serotonin. Neurotransmitters are a type of chemical messenger which transmit signals across from one nerve cell to another.
Dopamine brings feelings of pleasure and provides a happiness boost based on a certain action. Vital brain functions that affect mood, sleep, memory, learning, concentration, and motor control are influenced by the levels of dopamine in a person’s body. A dopamine deficiency may be related to certain medical conditions, including depression and Parkinson’s disease.
Serotonin is more of a mood stabilizer than a booster. The non-mood related functions of serotonin and dopamine also differ, as dopamine primarily controls movement and serotonin contributes to sleep and digestion.
What can help alleviate the symptoms of mild to moderate depression on the PKU diet?
- Socialise with others in the community, as well as with family and friends outside of the PKU community. Interaction will combat feelings of isolation and loneliness. There are lots of events held throughout the year, across the UK, as well as the NSPKU’s annual conference.
- Connect with the community online through social media. You might be the only PKU person in your village, but there is a huge network out there! Some suggestions: PKU UK & Ireland, PKU Worldwide Support Network, NSPKU, Low Protein In 15.
- Join the gym or start to walk every day as part of your routine. Exercise can have a massive impact on how you view yourself and how you feel mentally.
- Stay on a low protein diet and keep your Phe levels consistently low as directed by your dietician. The more volatile your levels are, the higher the risk of constant tiredness, sadness and low mood.
- Make sure you discuss low mood with your PKU clinic as they are the experts in your treatment.
For more information, contact us on ukinfo@cambrooke.com.

History of the PKU Diet
History of the PKU Diet
The first detection of PKU can be traced back to Professor Følling in Norway in 1934. The parents of two children that were not developing as they should, took urine samples to Følling, their physician, and large amounts of phenylalanine were discovered. It then became Følling’s mission to test the urine of children showing similar developmental issues across the country. Over 400 children were tested and high levels of phenylalanine were detected prevalently throughout several of the subjects.
In 1936, Lionel Penrose was the first to use ‘diet’ to treat PKU. However his initial diet of apples, sugar and not much else, caused malnutrition amongst his subjects as they were getting no protein or amino acid substitutes alongside this low protein diet.
Horst Bickel developed a treatment for Sheila Jones in 1951/2. Robert Guthrie developed newborn screening in the mid 1960s, and it was subsequently rolled out across the UK in 1969. Previously, a nappy test (urine test) was conducted on children from 1952-1969 in the UK as Følling originally had done in Norway in 1934. But it was not applied to newborns, was not very sensitive and was not done universally.
Both Bickel and Guthrie were born on the 28th June, hence why we now celebrate International PKU Awareness Day on this day each year.
The first child to be successfully treated in 1951, was unfortunately unable to maintain the diet at the time. However, it was the first time the low phe diet was deemed effective. The original diet consisted mainly of gluten-free wheat starch in water, orange juice, cabbage, turnips, butter, apples, cooked apples and banana. In 1963 the first PKU guidelines were released and registers began monitoring patient diet and uptake.
Over the years, the guidance on the ‘age’ for staying on diet has also changed. Diet only in childhood was seen as necessary in the 1960s, whereas today, ‘diet for life’ and ‘treatment for life’ are advised.
The age for staying on diet steadily increased as the IQ of PKU adults was consistently falling.
In 1960, the first manufactured protein substitutes were produced and the idea of ‘free foods’ was introduced. ‘Free foods’ are now called ‘exchange free’ foods, to avoid unrestrained eating within this food group. For example, sugary sweets might be a ‘free-food’, but if you ate them in excessive amounts, you could be susceptible to tooth decay, obesity and other health problems.
The NSPKU, consultants, dietitians, PKU researchers and companies, continue to push through studies to increase our knowledge of PKU and treatment.
Join the NSPKU to receive their members’ newsletter.

The PKU Diet and Pregnancy
The PKU Diet and Pregnancy
At Salford’s PKU day in May 2019, Diane Green took attendees through The PKU Diet & Pregnancy, providing information on how pregnant women with PKU can adapt their low protein diet to ensure their baby is born both happy and healthy.
The effects of blood phenylalanine on the offspring of women with phenylketonuria (PKU) were recognised in the late 1950s and 1960s. PKU mums require access to PKU diet protein substitutes, low protein foods and calorie supplements. During pregnancy, PKU mums also require Folic acid, vitamin D and EFA supplementation as per NICE guidance. Your dietitian can provide tailored advice for you.
Maternal PKU: A brief history
A 1957 study found that high phe levels in pregnant mothers, can produce foetal brain damage, and the research today sings from the same hymn sheet.
The importance of maintaining an even stricter PKU diet during pregnancy can’t be stressed enough amongst dietitians and consultants specialising in the dietary management of PKU.
From 1984-2002, the first Maternal PKU collaborative study took place. This study involved 416 pregnancies and monitored the Phe levels in PKU patients as well as the development of their new-borns into childhood.
Maternal PKU syndrome
Phe blood levels consistently over 360, have been found to contribute to Maternal PKU Syndrome, which can cause an unborn child to suffer from:
- Intellectual disability
- Low birth weight
- Microcephaly
- Congenital heart defects
- Miscarriage
- Facial dysmorphia
- And more.
Can pregnant mothers restrict themselves too much?
In a few cases, expectant mothers have been so keen to stay on their low protein diet, that they have gone too far in restricting protein and their baby has been born malnourished.
The baby still needs the building blocks of protein to grow into a healthy child, and protein substitutes or amino acid formulas can help facilitate that, as well as other supplements as recommended by your dietitian.
Unplanned pregnancies
For unplanned pregnancies, phe levels need to be brought into range as soon as possible to minimise the unborn child’s potential health issues. It is strongly advised that if you are living with PKU, you use multiple forms of contraception, to avoid potential harm.
Target Phe levels during pregnancy
European guidelines stipulate that Phe levels should be maintained in the range of 120-360 micromol/L throughout pregnancy to ensure your baby is born both happy and healthy.
Always consult your dietitian if you are thinking about having a child, to ensure the best outcome for your family and have the best guidance for your PKU diet.

International PKU Day
International PKU Day
Every year on the 28th of June, the PKU community joins together to celebrate International PKU Day. It’s one of the most talked about days in the PKU community calendar, and a time where families, patients, charities and companies join together to raise awareness of Phenylketonuria.
Raising Awareness
A brief chat with different people in the PKU community will show you that International PKU Day means different things to many of us. We feel International PKU Day serves its biggest purpose to PKU families by acting as an annual encouragement to raise awareness of Phenylketonuria.
Many people within the community take part in fund raising activities, share their very own personal PKU stories (all packed with emotion) and broadcast the existence of PKU to the world. This year, the NSPKU have organised a Step forward for PKU walk on Sunday 30 June in Durham.
PKU is such a rare disorder, so its huge to make ourselves known to the rest of the world, not only to help raise funds for research, but also to help in a political struggle for PKU treatments to become available in the UK (which are already available elsewhere in Europe).
Remembrance to Robert Guthrie and Horst Bickel
International PKU Day also serves as a remembrance to two men who were born on 28th June. Robert Guthrie, born 28th June 1916, developed the first new-born screening test, and Horst Bickel, Born 28th June 1918, was the first to develop a low protein diet for PKU infants in 1951.
Without these amazing findings from Robert Guthrie and Horst Bickel, those with PKU would almost certainly be subject to mental retardation, with untreated new-born babies being dangerously affected by protein in foods and milk.
Anybody born with PKU genuinely owes their quality of life to Guthrie and Bickel, and their mutual birthday is certainly a fitting occasion to celebrate PKU as a successful, life changing discovery which the whole community is indescribably thankful for.
A Reason to Celebrate
With the raising awareness and remembrance of the two men who discovered a successful low protein diet for PKU, we really feel that International PKU Day gives us something to celebrate.
Some members of our tight-knit community might be celebrating by running a half marathon to raise money for PKU, others might bungee jump off a bridge or do a skydive, but getting together to enjoy the company of other people who also share the same day to day challenges is golden to those who live the PKU lifestyle.
There has never been a better time to get involved in raising awareness of PKU. Start a fundraising campaign in your community, talk to your local press, share your PKU story with the NSPKU or ask your friends, family and local MP to join the NSPKU’s Diet for a Day Challenge.
What does International PKU Day mean to you, and how are you going to get involved? Let us know in the comments!

PKU – What is happening inside you?
PKU – What is happening inside you?
PKU is the best known of the rare inherited metabolic disorders. It is caused by a genetic deficiency of the enzyme needed to convert one essential amino acid (phenylalanine) to another (tyrosine). It results in too much phenylalanine and not enough tyrosine.
PKU can cause profound effects on brain chemistry, a lack of essential blocks for other things (e.g. melanin, thyroid hormones) resulting in an IQ of around 30, agitation, and pale skin and hair, if not treated with a low-protein diet.
At Salford’s PKU patient event in May 2019, Consultant Gisela Wilcox delved into the effects of too much phenylalanine and not enough tyrosine in the PKU diet:
Effects of too much phenylalanine:
- Toxic effects on nervous system
- Oxidant stress and inflammation in brain and bone
- Decreased brain growth, remodelling, changes in white and grey matter
- Low bone density and fractures
Effects of too little tyrosine:
Tyrosine is an amino acid. Amino acids are the building blocks of protein. The body makes tyrosine from another amino acid called phenylalanine. Reducing phenylalanine therefore has a direct effect on tyrosine levels.
- Lack of dopamine in the brain – less drive, motivation, tired, poor concentration
- Tremor
- Pale hair and skin
- Decreased protein synthesis (skin/hair changes)
- Lack of thyroid hormones (bone development/energy)
More information
Read more about PKU and low protein diets here.
We hope this article was useful. If you have any further questions, email us at ukinfo@cambrooke.com.

About the NSPKU
Introduction
The NSPKU was founded in 1973 by Brian and Sylvia Smith, whose sole aim was to help build a community around Phenylketonuria (PKU), a rare metabolic disorder.
1 in 10,000 babies born in the UK have PKU, that equates to around 60-70 babies per year, and the NSPKU exists to support patients, families and carers and to help them live and thrive with the condition.
How can they help you?
The NSPKU has many functions, including but not limited to, promoting care, providing new parent packs, holding PKU events and conferences, and creation of advice papers for employers, pharmacists and professionals. All with the aim of keeping you on track with your low protein diet.
The organisation also sponsors medical research into alternative treatments and field a plethora of enquiries on a daily basis through social media, email, phone and direct message. Queries relate to anything from ‘travelling with PKU’ to ‘exchange value confirmations’ to ‘general support and guidance’. All queries are logged, tagged and followed up on.
The NSPKU have also been involved in raising awareness of PKU amongst MPs, and recently got a selection of MPs to do the PKU diet challenge for one day. As of 24 May, 2 of the MPs are looking to do the diet for a full week.
6 Demands for Change
The NSPKU have several objectives for the foreseeable future:
- All children and adults to be treated within specialist metabolic centres with experienced physicians and dietitians
- All adults with PKU to have lifelong systematic metabolic treatment and follow up in a specialist centre
- Fair, transparent and equitable commissioning of all non dietary treatment for PKU
- All patients to have BH4 responsiveness testing
- All patients should have access to psychological support and age appropriate neurocognitive testing and follow up support
- Better access to the full range of prescription products including low protein foods and protein substitutes.
NSPKU Annual Conference
The NSPKU’s annual conference is an excellent way for patients and new parents to find out everything they need to know about PKU and we would highly recommend attending. Over the three-day event, you will meet others with PKU in the UK, get food and recipe inspiration, try a range of protein substitutes to find the right formula for you, and attend talks from professionals in the field. These talks range from medical professional’s PKU research, to patients talking about living with PKU.
Comprehensive Food Guide
The NSPKU also maintain a very important ‘traffic light’ food booklet. ‘Green foods’ listed in the booklet are exchange free and do not need to be counted as exchanges. ‘Amber foods’ can be eaten in moderation but do need to be counted as exchanges. ‘Red foods’ should be avoided completely. All of our Low Protein in 15 recipes use exchange free foods from the green list unless explicitly stated.
If you have any other questions, email us at ukinfo@cambrooke.com.

The PKU Diet and Emotional Health
The PKU Diet and Emotional Health
At NSPKU 2019, Lesley Walker, Psychological Therapist, took attendees through her emotional first aid toolkit for combatting distress and trauma associated with living on a Low Protein Diet. We wanted to write a blog post about the main technique she uses for her own patients, to help others that might be going through similar emotional health issues.
Lesley’s children, son-in-law and grandchildren have PKU, so she knows first-hand how the condition can affect an individual and family.
Lesley likened the initial PKU diagnosis to a ‘trauma’. A trauma is an event that is (i) negative; (ii) life changing; and (iii) unexpected. Post traumatic stress disorder (PTSD), anxiety and depression can all result from this trauma if not addressed properly, and Lesley discussed her most effective technique for combatting these negative feelings. This technique is called the Emotional Freedom Technique.
The Emotional Freedom Technique: Introduction
The Emotional Freedom Technique (EFT), is a technique that has been used quite prevalently in the last 15 years, for combatting trauma. EFT is described as emotional acupuncture, without the needles.
According to Lesley, “If we are stressed, angry, fearful, phobic or anxious then our mind and body system goes into the fight or flight stress response. If this response is ongoing we often become worn out, sick, overweight and generally unhappy. This is when tapping becomes an extremely useful and effective technique. If used correctly it stops this stress response. Scientific studies have shown that using EFT, retrains the limbic system and permanently alters the brain’s neural pathways. In other words, it literally rewires the brain so that a previously negative event is perceived in a completely new, more positive way.”
The Emotional Freedom Technique: Initial task
First of all, you should list certain memories that triggered unpleasant feelings for you in the past. These could include: initial diagnosis, being at school, eating out, dealing with hospitals and medical professionals, entering teenage and more.
Then, list the emotions that come along with those memories. This could include: disbelief, loss, fear, responsibility, feeling different, isolation, lack of control, worry, guilt and so on.
The Emotional Freedom Technique: ‘Tapping’
Don’t attempt to fix all negative feelings at once. First of all, just focus on fixing one particular memory, and the corresponding negative feeling associated with that memory. Start small. Perhaps think about one negative problem or event that has been on your mind. Be very specific.
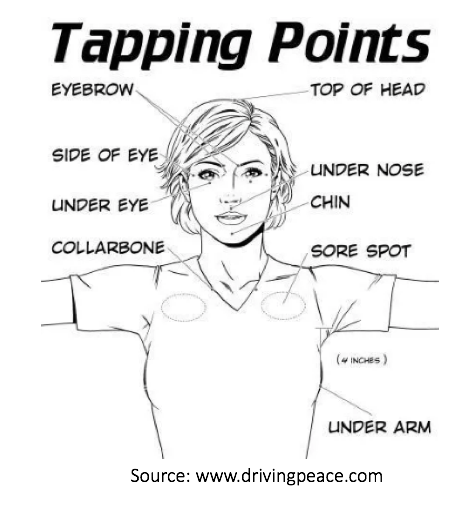
Using the three middle fingers on your right hand, lightly tap the side of your left hand (next to your baby finger) 10 times. Using the same three fingers, tap the top of your head, under your eye, under your nose (above lip), your chin, your collar bone, under your arm, and then repeat again (10 times each) for as long as you can or need to feel less stressed and more revived.
The Emotional Freedom Technique: How it works
Lesley claims that one hour of tapping has the ability to turn on/off 70 different genes. She also claims that the same hour of tapping can drop cortisol by as much as 24%. Cortisol is a stress hormone released by the adrenal glands, and is important for helping your body deal with stressful situations. However, too much cortisol, over time, can result in high blood pressure, weight gain, moods, reduced energy levels, poor sleep and more.
Tapping is based on acupuncture and is a form of ‘acupressure’. When ‘mind’ techniques fail to work, ‘body’ techniques are used as a more aggressive form of trauma relief, and have a much higher success rate.
If you have any further questions about this technique, the low protein diet or would like to speak with Lesley directly, visit: http://www.lesleywalkertherapy.com/. Or if you have any other questions, email us at ukinfo@cambrooke.com.

Siblings Day
Raising PKU and non-PKU siblings under one roof and at one dinner table can have its challenges
In honour of Siblings Day, we spoke with Kelly Thompson, Mum to Lily-Mae, 7 and Alan, 8. Lily-Mae has PKU and her big brother Alan was born without the condition. No other members of Kelly’s family have PKU, and when Lily-Mae was first diagnosed, it was difficult for Kelly to comprehend exactly how it would impact their lives.

What was it like for you when you found out your daughter had PKU?
I remember when I first got the call. I had no idea what PKU was, and even after driving 37 miles to the hospital, and speaking with the doctor, I felt none the wiser. I had never heard of anyone having this condition, and it just didn’t seem real. I remember calling my partner and asking him to speak to the doctor, so he could help explain it better to me, and it helped to talk it through with someone else.
I spent the next few weeks researching ‘PKU’ online, and then joined some UK and Ireland Facebook groups, which gave me food tips and I could ask more questions that I didn’t feel I could ask the doctor or dietician.
7 years on, and I am still learning something new every day.
How did your non-PKU child, Alan, initially respond to his sister eating different foods?
I distinctly remember Alan, at the age of two, running in shouting ‘Mummy, Mummy, Lily-Mae has taken my chicken nugget!’. That was my first recollection of him understanding that his little sister couldn’t eat certain foods.
Alan has always been very caring and has always looked out for his little sister. He will never tempt her with foods and they rarely fight or argue, and if they do, it is never about food.
How did you explain PKU to Alan, your non-PKU child?
I told Alan that Lily-Mae couldn’t eat some foods, as she would become poorly, and that was a good enough explanation for him.
I have not really needed to explain it to him again, as he sees me preparing different food for each of them, and it is just part of our life, so he rarely questions it.
Do you remember when Lily-Mae first understood that she couldn’t eat the same food as you and Alan?
We went to Cornwall in 2016, when Lily-Mae was four years old. A lady came over and asked if we all wanted a bacon sandwich, and before I could speak, Lily-Mae said ‘I can’t eat that, I have PKU’. And that was that – she had picked it up without us even having to tell her.
Tell us about meal times!
I always cook Lily-Mae the same food as us, only without the meat and with low-protein alternatives for the pasta, rice or bread. That way, all of the plates look the same, and she never even thinks twice about it.
To give you an example, we can get PKU friendly garlic bread, which Lily-Mae loves and so myself and Alan will have regular garlic bread, alongside rice (low protein for Lily-Mae) and bolognaise (veggie for Lily-Mae/meat for us).

What about when you go out? Does Lily-Mae find it hard when Alan can have anything he wants and she has limited choices?
Sometimes she wants something she can’t have, and instead of focusing on the thing she can’t have, we show her all of the things she can have. Making a positive from a negative always helps. For example, at the Zoo yesterday, Lily-Mae wanted a Calypo Duo, which was half milk, and I said ‘Oh look, they have Twisters! Yey!’ And she was content with a Twister. It is all about how you word it!
Does your non-PKU child ever feel left out, or of second importance?
I am very lucky that Alan has only ever wanted to help me look after Lily-Mae and police her eating habits, if they are staying with family or friends. Alan proudly tells everyone that his little sister has PKU, and when they respond with ‘what is that?’, he loves to explain what it is and what food she can and can’t eat. It can be quite the talking point!
What would be your advice to new parents of a child with PKU, who may have older non-PKU sibling(s)?
I only just found out about NSPKU and all of the support that they can provide. A few people from this organisation have helped me immeasurably. I also think that online support groups are great to provide answers to any questions that you might have about food and recipes.
I would also say that it is really important to talk about PKU openly with your affected child and their non-PKU siblings, so it just becomes a way of life. The more you talk about it day-to-day, the easier it gets.






